My Parkinson's data - at last!
Now I know the drugs do work - unless I have a cooked breakfast
For more than four years now I have been on a quest, searching for something that we are often told is the new oil. Yes, it is data I have been seeking - hard numbers about my Parkinson’s. How severe are my symptoms, do they vary throughout the day, do they respond to the medication I take?
The only time I get some vague snapshot of my condition is when I visit my excellent consultant at Charing Cross Hospital. He puts me through a series of exercises, pulls my limbs this way and that, and then, using his skill and judgement, comes up with what is called a UPDRS score. He then tweaks my medication but neither he nor I know what impact that has had until we meet again, which can be up to nine months later.
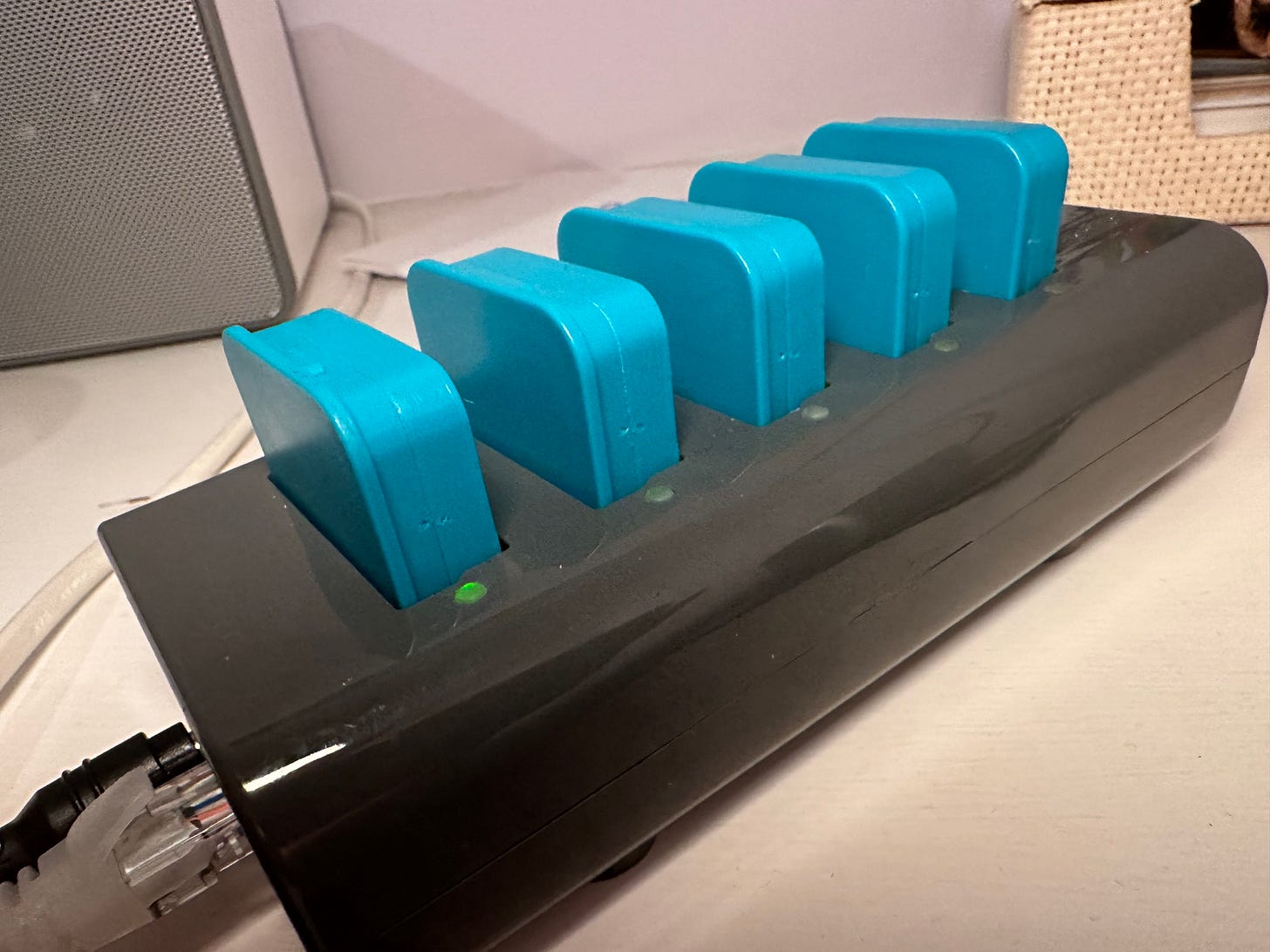
But now that has all changed. My doctor and I are both in possession of a 30 page document full of charts, numbers and facts about my Parkinson’s symptoms as measured during a week in June. The data comes from a company called PD Monitor and is the result of readings from five sensors, one worn on each limb, one around my waist. I strapped them on each morning, then each evening slotted them into a unit plugged into my router which recharged them and uploaded their data to the company’s secure cloud.
By the end of the week, I was finding the process of strapping on the sensors quite wearisome, especially the leg sensors which drew cracks from friends about my “tag” and when was I going to be set free. As well as being relieved when it was over I wondered whether it had been worth it when I knew something much simpler and less intrusive, an Apple Watch app, was available.
All of that changed a week later when Becky Duong, a neuro physiotherapist who now works for PD Monitor, came to my house to talk me through the data which had been supplied to my neurologist.
First, there was a list of symptoms and how much time they were present. I do have a tremor in my right arm which becomes more pronounced in moments of stress - I was driving during the last hour of the Test Match on Sunday and thought I might have to stop, so violently was my arm shaking. But PD Monitor says that is rare and the tremor is present just 1% of the time.
By contrast, Bradykinesia - slowness of movement - was in evidence 85% of the time I was wearing the sensors. I was taken aback by that - until I remembered how shocked I had been recently when I saw video of myself walking. Almost without noticing I have developed the Parkinson’s shuffle.
There were any number of charts detailing what each sensor measured but the one which painted the most interesting picture was the first one which you can see at the top of this post. This depicted my “off” score at half hour intervals throughout the day. When I was first diagnosed with Parkinson’s I struggled with the concept of “on” - when your medication is working - and “off” when it is wearing off, and your symptoms become more pronounced. I couldn’t really tell the difference but lately I have begun to notice just before I am due to take a pill that I am beginning to fade.
And this chart with the blue horizontal lines marking the times I take my pills told that story. The top half of the chart has half hour blocks for each day, coloured from light green (totally on) to dark pink (totally off). The bottom half sums up the average readings over the week with a line which soars when I am “off” and falls back when I’m “off”.
The reassuring message from this chart is that the drugs do work - the line rises as the time for me to take my next dose approaches, and falls afterwords. And there are some fascinating insights to be had by looking at the granular detail. It is between 10 and 11am that my “off’ score most often peaks, particularly on Saturday and Sunday, where there are two pink cubes.
That may be because at the weekends I often cook a big breakfast - scrambled eggs and bacon. I have been warned that eating protein too close to the time you take your pills makes it harder to absorb the medication and it seems here’s the proof. So will I mend my ways? Well, yes, I’ll get up early to take my drugs. I’m not giving up the weekly fry-up.
But overall, the data gives a positive message. A while back, my neurologist prescribed a top-up at noon and bedtime of the dopamine replacement Sinemet in a slow-release form. That seems to have done the trick of smoothing my path through the second half of the day - and without the dyskinesia (sudden jerky movements) which can be a side-effect of these drugs.
This kind of technology is going to be increasingly vital as we move towards a remote monitoring and home-based care system. I can see a few problems with it - some patients may find that wearing the sensors is just too much hassle, and the sheer volume of data generated by PD Monitor could make some neurologists feel even more overwhelmed.
But my doctor and I came to the same conclusion - by email - that my current drugs regime was about right. And if we do decide to change it, I can put on the sensors again and see how my body responds. I think I may have seen the future of Parkinson’s care…


Very interesting, thank you. A clear pointer to the direction of travel for care, with continuous, sensor-driven monitoring and AI-driven analysis to help titrate treatments &/or recommend specialist interventions. One issue I foresee is that we will wish to have as few sensors and apps as possible for all of our co-morbidities, which will require some higher level co-ordination. I should declare that I have an interest in the field with my Board position representing Parkwalk Advisors as investor at Charco Neurotech.
I do think that the combination of drugs, sensors and access to data is going to be a big thing for medicine in the future, allowing patients with chronic illnesses to tailor the regime to their own lifestyle. I love the idea of moving the medicine time so that you can continue to enjoy the fry-up. That puts you in charge.
Big hugs to #sophiefromromania 😍