How do you begin to tackle the immediate crisis facing the NHS, the huge waiting lists that stubbornly refuse to come down, so that the focus can switch to long-term goals? The obvious answer is more cash, and we can expect the health service to be among the few winners from Rachel Reeves’ budget next week.
But this week I have heard a couple of things which have made me wonder whether there might be simple and relatively cheap ways of tackling waiting lists. The first was a tweet from a health journalist Alison Moore:
“What? Waiting times reduced from a year to 7 weeks by employing an administrator,” she wrote. With the tweet was an extract from a document describing how in East Sussex a new booking system for children’s therapies services, with a business manager taking over the administrative work from doctors, had resulted in a dramatic fall in waiting lists.
Later, the Kent Community Health Trust, which runs the East Sussex service, said the new administrator was just one of a number of improvements to the system which had reduced waiting times, but said its overall ambition involved “freeing up our clinicians so they can see more children, rather than spending time on admin tasks which can be completed by someone else on the team.”
The Trust says this is “not rocket science” and that is true . Across many industries there is a growing backlash against the idea that, just because computers allow anyone to undertake tasks they used to leave to admin staff, highly skilled, highly paid people should waste their time doing them.
But still the myth persists that the NHS’s problems could be sorted out if most of the managers were sacked and the frontline medical staff could be left to run things. You might question whether the NHS has got the right mix of skills amongst its managers and administrators but at just 3% of the workforce, the problem is that there are too few of them, not too many.
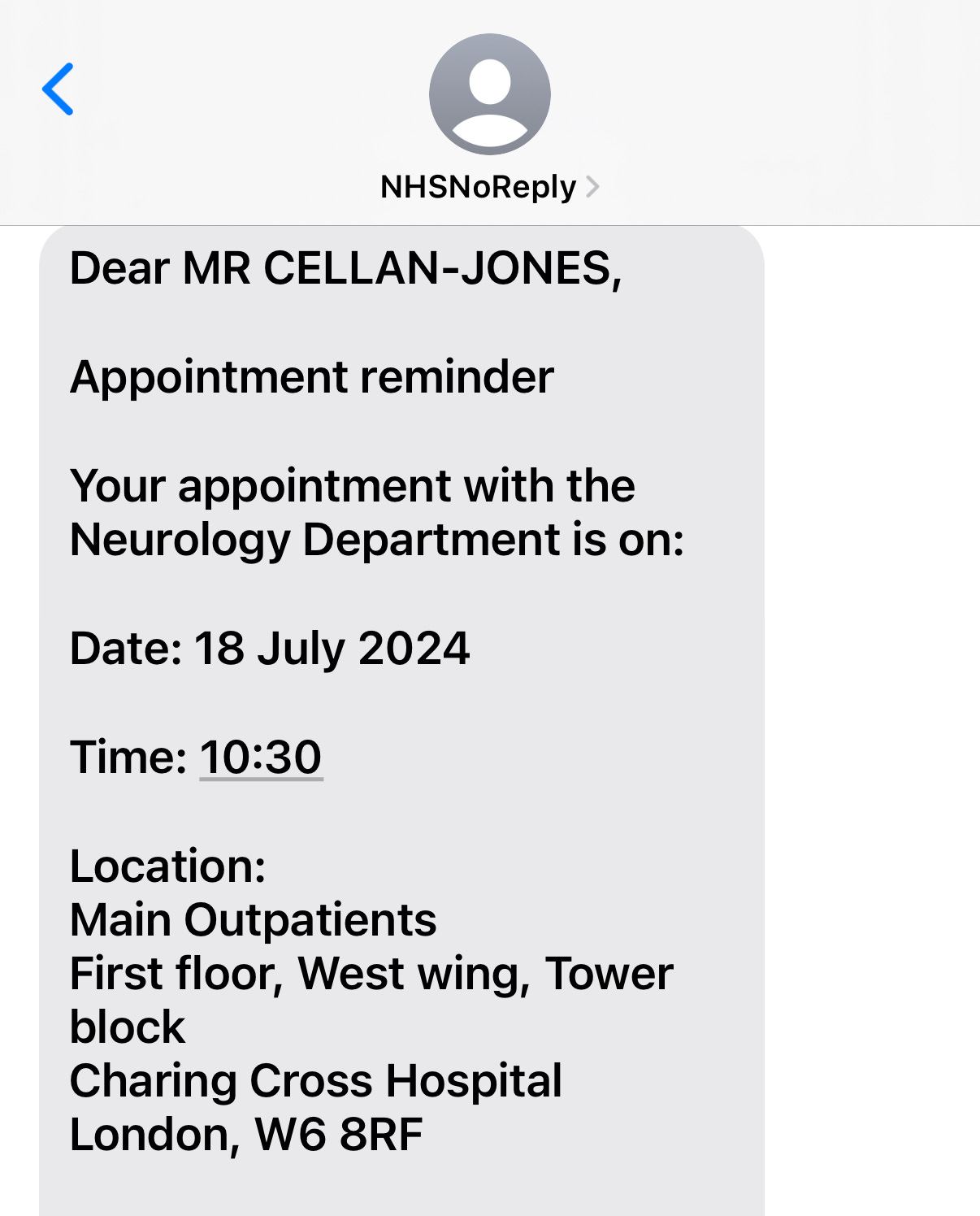
The second illuminating thing I heard this week was a report on an issue which might sound trivial but causes a lot of waste right across the NHS. The acronym DNA - ‘did not attend” - is used to describe a missed hospital appointment and according to DrDoctor, the digital appointment service behind the report, there are 46 DNAs every minute.
“It's a £1.6 billion a year problem for the NHS,” says Tom Whicher, CEO of Dr Doctor, putting the problem in the context of the waiting list. “It's still seven and a bit,million people, which almost exactly matches the number of missed appointments every year.”
The survey quizzed 5,003 people who missed at least one hospital appointment over the last two years. 42% of respondents admitted feeling anxious in the run up to an appointment and the kind of people who miss appointments once are likely to do it again. Asked which kind of appointments they were likely to attend, 72% said they would turn up for a gym session, compared to just 57% who said they’d get to their hospital appointment.
Transport appears to be a major issue - 50% of respondents blamed issues ranging from being sent to hospitals too far away to the cost of travel for their non-attendance. Issues with getting time off work or fear of losing income were blamed by 27%. While in my experience both hospitals and GPs are now good at pushing out reminders of upcoming appointments via text and email, 29% of patients said they had tried to rearrange their appointments but had been unable to get through to anyone on the phone.
So what’s to be done? Stories that Health Secretary Wes Streeting has floated the idea of fining patients for missing appointments have been rubbished by the government and Tom Whicher says that would be a bad approach.
Instead, he has some ideas to deal with an issue which he says is perfectly solvable. First is to make sure all hospitals send out those text reminders I mentioned. “If you send a text message notification to patients, you typically reduce “did not attends” by 30% straight away.” It seems extraordinary to me that any hospital has failed to bring this in already, but apparently some are still stuck in the last century.
Second is giving patients some choice over the scheduling of their appointments. “The classic that we see is you give someone a 9am appointment and they're going to come by bus, and the buses don't start in time for them to get there,” says Tom. He says giving patients a say over the timing of appointments has a dramatic effect: “In clinics where patients choose their own times, the DNA rate tends to run at about 4% as opposed to 7 or 8%.”
He also wants to see more of what is called dynamic booking, where instead of telling everyone at a clinic that they will be seen again in six months, patients are contacted a few weeks before they are next due an appointment, and invited to book themselves in. “It's a higher overhead process, but you get much higher attendance rates, and you get much, much better clinical safety.”
Finally, Tom Whicher believes that AI can help - and you won’t be surprised to hear that DrDoctor has developed its own solution:”We've built this tool which takes an individual and it says for that individual and their age and their demographic group and their co-morbidities and their past attendance history, we can predict the likelihood of them coming or not coming to a certain appointment, and then we can proactively intervene.”
This proactive intervention turns out to be quite old-fashioned, a phone call to the patient to remind them about their appointment. and talk them through the reasons it is important that they attend I suggest that the recipient of such a call may feel offended at the suggestion that they are likely to be a no-show, and Tom explains that the caller will be a little more subtle than that.
So what is his evidence that this programme of relatively simple tweaks to the appointments system can be effective? He says while the national rate of DNAs is 11%, good hospitals which have implemented these ideas have got their rate down to 3 or 4%.
Now, these kind of initiatives often generate good results at first when the idea of text reminders or scheduling your own appointment is new, only to disappoint when they become familiar. But let’s not be defeatist - mending the NHS is going to take a monumental effort from the clinicians, the managers, and yes, we the patients. So let’s be positive about small things that can make a big difference - like turning up at the right time for an appointment.



Great ideas, affordable, now let’s implement before the newest health secretary decides he wants to try his own ideas out. We all know how tgat goes.
Yes agree with all those ideas and sure they would make lots of significant improvements if introduced. However there are just as much waste in the private medicine world that could help speed up the process and make efficiencies.
It's impotent to take the best suggestions from both sides and then incorporate them quickly.
Keep up the good work Rory always appreciate it what your doing.