Can Neu Health Transform Parkinson's Care?
A smartphone app which could bridge the gap in treatment
In my career as a technology journalist one thing excited me more than just about anything else. No, not talking to Elon Musk or being there when the iPhone was launched, but meeting hopeful startup companies with ideas that promised to change the world. Now, most of them subsequently vanished without trace but a few - and notably the barebones computer Raspberry Pi - surpassed even their founders’ hopes.
When I met via a video call two of the founders of Neu Health, a startup spun out of Oxford University, I got that buzz again. Perhaps it was because the business is aimed at something right at the centre of my interests, transforming Parkinson’s care using smartphones.
Caroline Cake, Neu Health’s Chief Executive, and Dr Kinan Muhammed, Co-Founder & Chief Medical Officer, outlined their plan to let patients and their doctors monitor the progression of Parkinson’s via an app. The company has only been going for a year but it builds on a decade’s work by another co-founder Professor Michele Hu, whose Oxford lab has been working with hundreds of Parkinson’s patients, and with Dr Muhammed, a consultant neurologist and Oxford academic focused on digital health. They have developed an app which uses a smartphone’s sensors to allow the patient to measure a whole range of Parkinson’s symptoms:
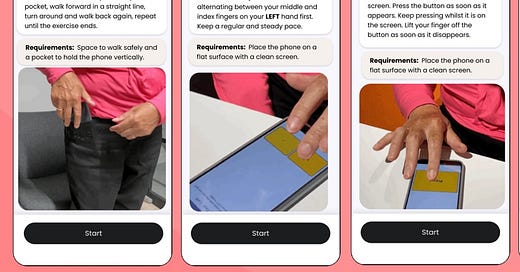
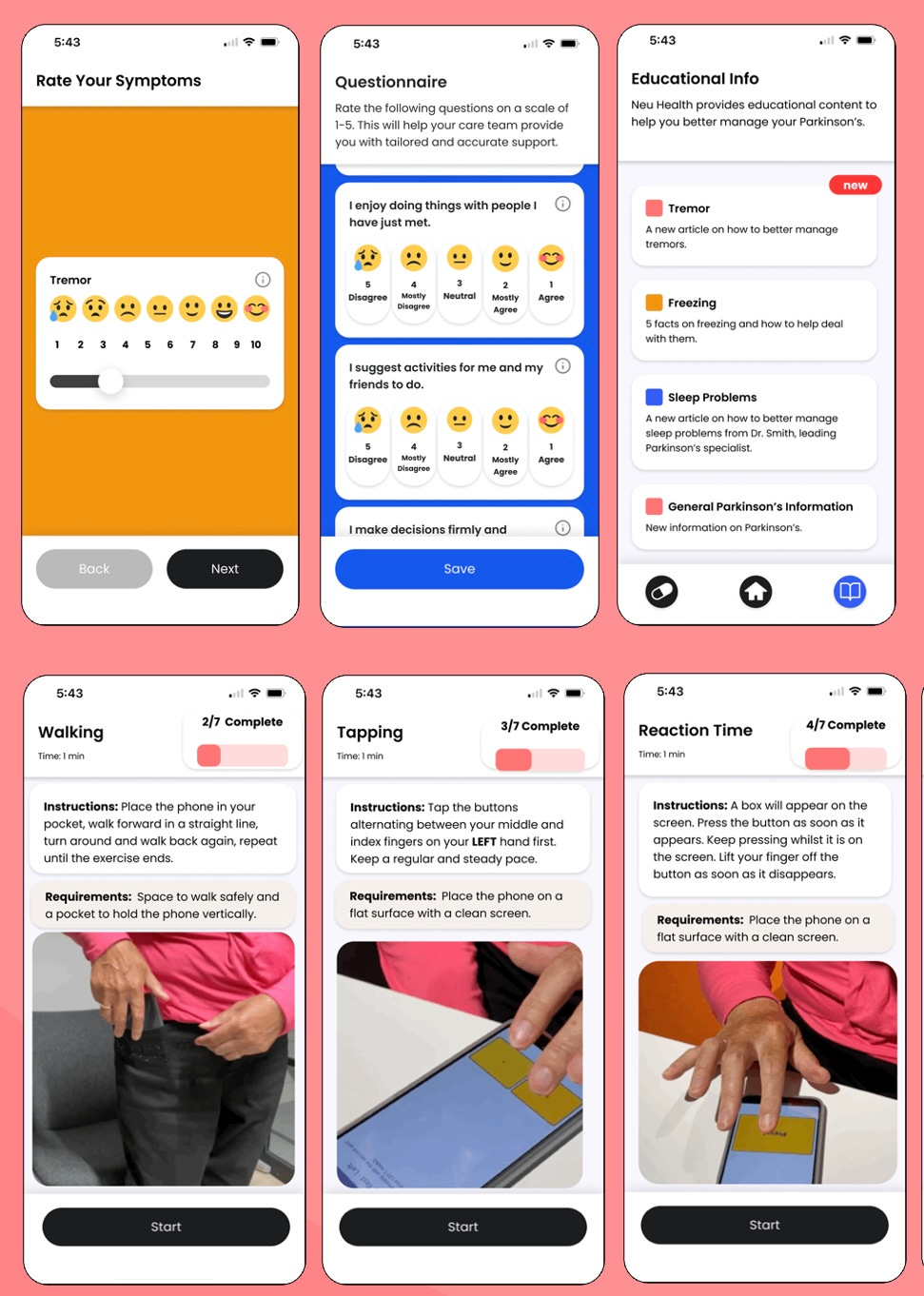
“They include things like measuring voice, so you'd hold the phone and just say “ah” into the phone,” explains Kinan Muhammed. “It can measure tremor, both rest tremor and postural tremor, reaction speed, walking balance and cognitive function as well. There's a whole host of stuff that you can measure all remotely on the phone.”
They have then done clever things with the data collected by the phone: “A number of algorithms were developed that let you estimate clinical scores that are otherwise very subjective and take about an hour to do if you were to do it in clinic whereas actually the numbers can be generated straight away.”
I have written before about the huge challenge of measuring Parkinson’s symptoms, still mostly done by your consultant getting you to.walk up and down the corridor, get up from a chair, open and close the fingers of one hand and a series of other exercises to end up calculating what is known as a UPDRS score. If technology can be developed to automate this process - and Neu Health is just one amongst a number of companies trying to do this - then all sorts of good things will happen.
Drug trials will be easier and faster to run, with participants able to upload readings of their symptoms remotely rather than needing to turn up at a hospital or clinic, and a more precise measurement of the impact of a drug should lead to faster decisions on whether or not it is worth taking it to the next stage.
That ability to monitor patients remotely promises a wider revolution in Parkinson’s care and this is where Neu Health is focused. While other similar projects are using smartwatches or, like the PD Monitor I tried out, a whole range of wearable sensors, the Oxford-based company is trying to make things simple for both patients and doctors: “We're trying to keep it on people's own smartphones<“ explains Caroline Cake, “so from a clinical point of view, there's not a lot of equipment you're having to send out.”
The idea is that Neu’s app can help bridge the huge gap in Parkinson’s care, the period between neurologist appointments which can last a year or more. Dr Muhammed makes the point that even when you do get to see the doctor, the brief appointment is taken up with getting a snapshot of your symptoms that day. “Whereas what we're trying to do here is allow them to have all that information on a dashboard, so that before you've even walked through the door, they know what's been going on. They know what your priorities are because you've listed them and you can change it. And then they can spend time actually working with you to optimise medication.”
When he shows me a mockup of the dashboard one thing stands out - a chart showing the doctor not just what is happening to the patient now but what may happen over the next 18 months. Kinan Muhammed explains that the clinician can find answers to various questions:”What is the chance of this person actually seeing disease progression? What's the chance of them having a fall and the chances of having cognitive decline?"
The system is now being tried out by the NHS in Suffolk. The app has been cleared as a medical device and its registration accepted so the trial is more about whether it provides value for money than its safety or effectiveness. A system where people with Parkinson’s can have their symptoms monitored remotely so that, for instance, early warning can be given if a new medication isn’t working, sounds like the future. But in the short-term bringing in new technology and training staff to use it can be expensive.
So Caroline Cake is hoping that potential customers will be looking at the longer term and asking themselves what benefits the Neu app could bring:
“Can we reduce the likelihood of admissions to hospital, can we reduce the length of stay when someone is in hospital because there's this kind of programme of care around them?”
For new technology to produce tangible benefits, organisations often have to radically rethink the way they work, in the face of resistance from those who cry “but we’ve always done it like this.” If companies like Neu Health are to transform healthcare, then we are going to have to hope that there are enough radical thinkers in the NHS to allow it to embrace change. .


My father had Parkinson's towards the end of his life compounded by severe rheumatoid arthritis. The care & advise we received was minimal - this was between 2000 - 2007. I now know I could smell Parkinson's - I loved to cuddle dad & so I soon noticed the change.
The app sounds extremely interesting & I feel would have helped in dad's treatment. His voice in particular changed & was certainly a guage in his decline.
One if the issues I had surrounding dad's care/ treatment was because he developed the disease in his late 70s it was considered inevitable almost normal & because he had severe rheumatoid arthritis many symptoms were over looked - eg feet shuffling. It was my daughter that noticed he walked like a "Choo Choo train" years before formal diagnosis. In light of this I think there is a case for smart phones to collect medical data day to day to anticipate issues. Late diagnosis exacerbates problems in the elderly (as I'm beginning to discover now myself)
I hope you get chance to use the new tech - I know how powerful it can be as I completed my MA in Ed tech at London Knowledge Lab. All the best & take care