After The Fall - Two
The NHS needs to learn to talk to itself and others
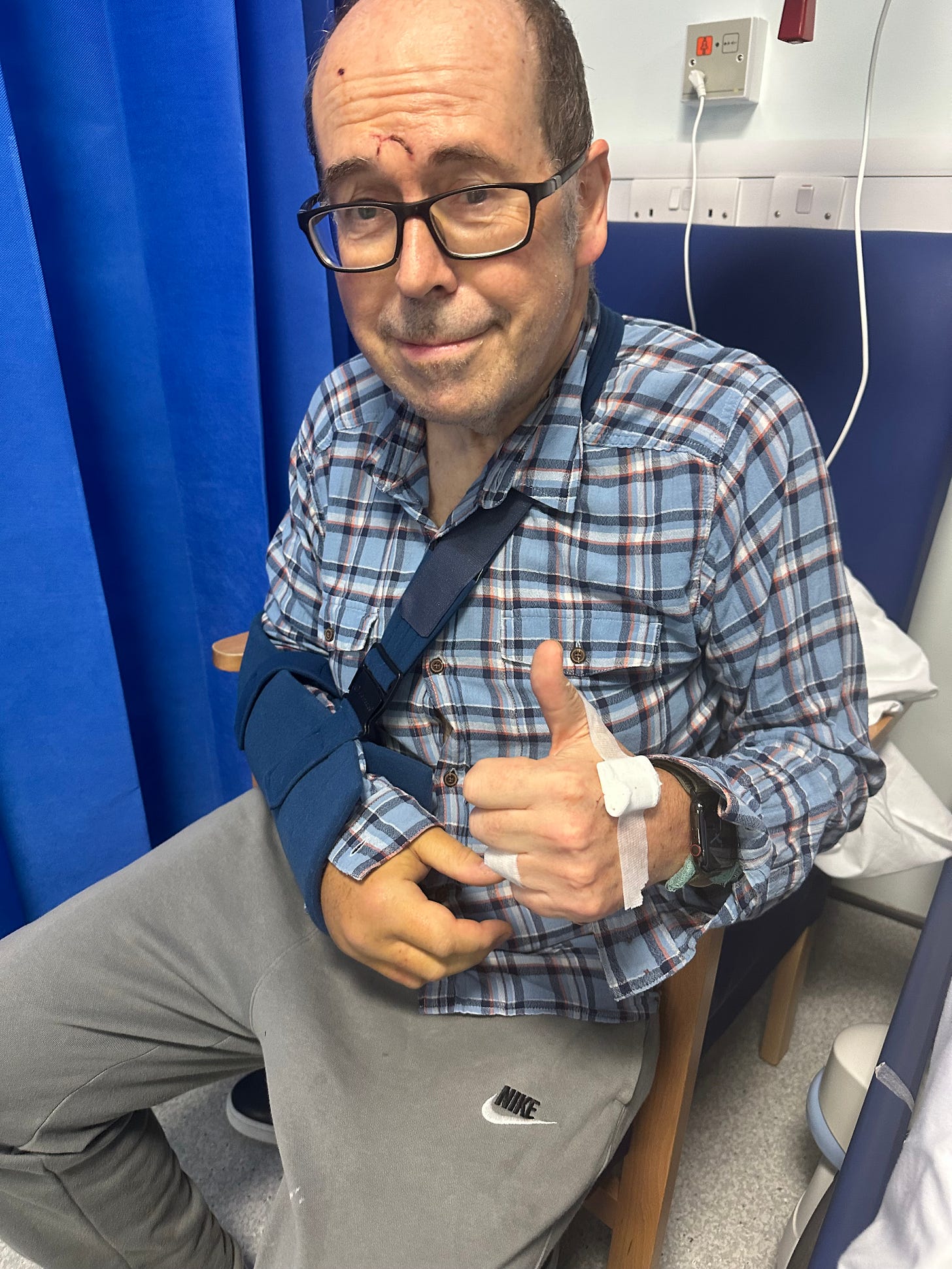
Last Monday I wrote about the fall which shattered my elbow and had quite a disastrous effect on my confidence. A week on, some of that confidence has returned and I feel that I am on the road to recovery. But before things got better they got a lot worse.
What follows is not meant as a complaint but as an observation from a patient of the importance of improving communications across the NHS.
I began last week anxiously awaiting a call from Ealing Hospital to tell me when they would be calling me back in for an operation on my fractured elbow. They had sent me home in the early hours of Saturday morning after first thinking that I might stay and have the operation over the weekend.
One source of anxiety was the difficulty of contacting anyone at the hospital. Without a name you are lost in switchboard hell, passed from one extension to another, as you try to identify the correct department. I received one call on Monday morning, telling me they would be in touch with an appointment time to come in - and then nothing.
Finally, at lunchtime on Tuesday a registrar rang asking me to pop in for a CT scan on my elbow. A kind neighbour dropped me at the hospital, the scan was done quickly and relatively painlessly, and I made my way home in a taxi.
But at 5pm my phone rang again, and it was the registrar sounding worried. The scan had shown what she described as gas in the wound, meaning it was an open fracture, where the bone has pierced the skin. This apparently made mine a more complicated case because of the risk of infection, and that should have been made clear in the notes when I was discharged on Saturday morning.
In fact, another junior doctor later told me I should not have been released at all, and there had been something of a cock up.
Anyway, the registrar now wanted me to return to the hospital to be admitted, put on an antibiotic drip, and prepared for surgery, either on Wednesday or Thursday.
At least that sounded like a clear plan of action, and when my wife Diane got home, we set off for the hospital. We arrived at 7pm under the foolish misapprehension that I would be whisked in and put on that antibiotic drip pronto. No such luck, it was 9pm before I was lying on a stretcher with the registrar inspecting my wound and replacing the plaster cast. We were in a cubicle which also housed the linen cupboard so there was a constant stream of medical staff coming through in search of sheets and pillows.
It was 1 am before they finally found me a bed on a ward. Now we all know about the pressures on A&E and the scarcity of beds, and the hard-pressed staff were lovely, so I could accept the long wait. What did worry me was exactly when I was going to be put on the antibiotic drip I had been told was so urgent. After the registrar had gone. I kept mentioning this to anyone who came near me but got blank looks. After 11 pm I was told I could no longer eat or drink so that I would be ready for surgery in the morning - but surely a drip would play a vital part in that? Finally, at 3 am a canula was inserted in my hand, and the antibiotics began to flow.
Wednesday morning came after a virtually sleepless night, but I felt positive because at last my fracture was going to be sorted out. Or was it? I kept asking when a decision would be made on my operation but got no answers. Hope began to fade and then around 1015 a doctor arrived and seemed surprised that I had ever expected to be heading to theatre - after all, I had only been on the antibiotics for a short while.
I felt a huge sense of anticlimax but at least I could have some breakfast now, and the hospital food was actually pretty good. I told myself that by Thursday afternoon my elbow would have been patched up - nobody had yet explained how - and I could head home to start my recovery.
The whole cycle began again - nil by mouth after 11pm, a few hours of fitful sleep, awake at 5.30 eager to go - but with the same result. At 7 am a doctor came and drew a big arrow with a black marker pen on my right arm, pointing at the elbow, which seemed a good sign. But I knew the decision about today’s surgery list would be made at an 8 o’clock meeting and when by 9 I had heard nothing I feared the worst.
At 9.30 I texted Diane:”Still waiting for information. This place is driving me nuts.” Shortly afterwards came confirmation – I had been bumped off the list. With limited theatre capacity Ealing has to prioritise the emergency cases and overnight an 94-year-old had broken his hip and someone else had been injured in a car accident. It was hard to argue that they should not be given priority. Nevertheless, if I had been kept in back on Saturday. I would have been sorted by now.
My misery plumbed new depths. While my Parkinson’s may not have caused my fall, my symptoms were now being exacerbated by the pain and discomfort from my right arm. These were the “good” early years after diagnosis when I felt I was coping reasonably well - now I feared I would emerge from this ordeal having taken a big step down the Parkinson’s ladder of decline.
To be fair, the hospital now appeared to understand my concerns. Suddenly I had three doctors and a senior nurse around my bed discussing the options. We could go again on Friday, although there was the risk of another emergency case, bumping me off the list, or I could go to another hospital Northwick Park where an upper arm surgeon had said he could treat me on Saturday. I was adamant that I wanted it done as soon as possible which meant going for the Friday option, but somehow a decision was made that I should go to Northwick Park,
After 36 hours occupying a valuable bed to no purpose I was released from Ealing Hospital to go home for the night – although going through the paperwork to allow my release took four hours.
But on Friday at home, there was more tension. I had been told to expect a call in the late afternoon from Northwick Park to confirm that I was on the Saturday list but warned there was still a chance that they might bump me too.
By 5.30pm there had been no call and my attempts to reach the orthopaedic team via the hospital switchboard had failed. “We can’t go on like this,“ said Diane, and we even began to explore whether I could have an operation from a private surgeon. Then her phone rang. It was a doctor from Ealing telling us that Northwick Park had been trying to contact us on our home landline number. This has been out of action for a while and why Ealing had supplied that number when they had been calling me on my mobile remains a mystery.
Soon I was in touch with Northwick Park and told to turn up at 7:30 on Saturday morning. My dear wife carefully installed me like a Ming vase in the car the next morning and drove the unfamiliar route through pouring rain to the giant hospital campus in Harrow. From then on, everything went smoothly. I first met the anaesthetist and then the two surgeons who explained in great detail what had happened to my elbow and what they were going to do to fix it..
I was first on the surgery list and woke shortly after 2pm in some pain, but hugely relieved that the job been done. That evening, Diane drove me home again through pouring rain and, eight days after my accident, my recuperation could begin.
I do want to stress that at Ealing hospital and Northwick Park I was treated by excellent staff working under great pressure in difficult circumstances. But what struck me is that the NHS remains a cumbersome beast that struggles to talk to its patients or to itself.
As a patient, getting information about one’s treatment seems like an obstacle race where the system is always one step ahead. Without the name of at least one doctor involved in your treatment - and preferably their email address – you will get nowhere. But communications between medical staff within and between hospitals also appear hopelessly inadequate, with the gulf between doctors and nurses particularly acute.
I also sense that in some cases new computer systems are slowing not speeding information through the system. On Saturday morning, as we waited in the Surgical Assessment Unit, four nurses gathered around a computer screen while a fifth explained to them all the steps needed in a program to check a patient in and get them into a bed. It took about 20 minutes and appeared to be akin to mastering some complex video game beset with bear traps.
One bright spot was the NHS app which was often first with new information, such as my discharge letter from Ealing Hospital, but I still had to wait for it to be printed out and brought up to the ward before I could go.
I am very grateful that the NHS finally came good and fixed me up, and I am slowly getting back my mojo as I prepare for the many projects which will keep me busy until Christmas. But my week as a customer of the health service has left me convinced that more money and more staff won’t solve its problems without some fundamental changes in the way it communicates.

It is alarming that two people like yourself and Diane who are so tech savvy and generally clued up were pushed around from pillar to post. Imagine being old and alone and encountering all this mayhem.
So sorry about the fall and hope you are now on the path to recovery.
You are spot on with communication. Doctors (mostly) seem to be culturally unable to communicate with patients and, almost more so, between themselves. The systems seem terrible, there is no overlap within institutions and woe betide you if more than one institution is involved.
One of the problems is that the patient is not valued (resulting in misallocation of resources) and often has no idea what is going on. This is much worse if the patient is really unwell or elderly and does not have someone to help navigate the system on their behalf. Doctors are often individually defensive, but this is nothing compared to the NHS as a whole.
The system does not listen to the patient. 'Letters' are a disgrace, taking weeks to arrive in some cases (the NHS must be the biggest user of the postal system!).
The NHS app is, as you say, a useful conduit and needs to be enlarged upon. The patients need to own their data, which would get around a lot of the privacy concerns. There is so much to be done!